
Tocolytics In Pregnancy
4 min readWritten by Editorial Team


Preterm birth is one of the most common and most expensive complications of pregnancy. As many as 11% of all pregnancies are complicated by it, and it is responsible for 70% of all sick babies. Some patients experiencing preterm labor may benefit from tocolysis, an obstetrical procedure that prolongs gestation. Different medications can achieve this by inhibiting smooth muscle contractions in the uterus. This blog has some information about tocolytics in pregnancy.
Preterm labor patients may benefit from short-term administration of tocolytic agents. It is advantageous to prolong pregnancy because it allows for other proven interventions, such as the administration of antenatal corticosteroids.
In This Article
- What are Tocolytics?
- Diagnosis of Preterm Labor and Tocolytics
- Tocolytics in Pregnancy
- Causes Of Preterm Labor
- Treatment of Preterm Labor with Toclytic Agents
- When Should You Not Use Tocolytics Medications?
- Side Effects Of Tocolytics
What are Tocolytics?
Tocolytics which are also known as labor represent drugs or anti-contraction medications are the drugs used to suppress the initiation of premature labor. These drugs help to avoid and postpone the premature delivery of a baby. The therapy helps buy time for a day or two for the administration of betamethasone, a glucocorticoid drug that greatly accelerates fetal lung maturity so that the baby can breathe on her own even after preterm birth.
The inhibition of uterine contractions is partial and tocolytic medications can postpone the birth for a few days at the maximum. However, they are not always very effective and sometimes delay the birth by only a day or so. Strict monitoring of blood pressure, fetal movements, etc is required while using tocolytic drugs.
Diagnosis of Preterm Labor and Tocolytics
The most reliable and correct diagnosis of preterm labor is based on clinical symptoms which are sometimes imperfect as preterm labor subsides in 30 percent of patients. The most reliable markers of preterm labor are painful, continuous uterine contractions accompanied by softening, dilatation, and effacement of the cervix. Cervical effacement is the thinning out of the cervix.
Tocolytics medications inhibit or suppress the contractions of myometrium. This is the prime focus of preterm labor. Tocolytics help in delaying preterm birth and prevent maternal and fetal risks as far as possible. During this delay, antenatal corticosteroids can be administered to lower the risk of respiratory distress in neonates.
The commonly used corticosteroids are betamethasone, dexamethasones and should be given at least 18 hours before the preterm birth. Antenatal corticosteroids reduce neonatal morbidities (intraventricular hemorrhage and necrotizing enterocolitis).
Tocolytics in Pregnancy
Never take tocolytics medications before 17-20 weeks of pregnancy to treat preterm labor. Some doctors prescribe tocolytics post completion of 34 weeks of pregnancy while others wait till the 36th week. Different agents of tocolytics are prescribed by doctors after assessing the risks and the benefits.
Tocolytic medications have been available for ages. But the knowledge about their role in the suppression of preterm labor comes out recently. Preterm delivery is delivery occurring before 37 weeks of gestation.
Causes Of Preterm Labor

It is unclear what causes premature labor. The premature activation of physiological contracting processes or pathological factors associated with uterine contractions can end up in preterm delivery. A compilation of factors responsible for preterm births consist of:
- Stretching and over-distension of myometrial and fetal membranes
- Activation of the placenta
- Decidual hemorrhage,
- Fetal placental hypothalamic-pituitary-adrenal axis
- Inflammation or infection of the uterus is
Additionally, preterm births are more common in elderly pregnant women, an increase in the usage of assisted reproductive techniques, and increased awareness of maternal health among physicians.
Treatment of Preterm Labor with Toclytic Agents
The tocolytic drugs can slow down contractions. Following classes of tocolytic agents are widely available:
- Beta-mimetics (such as terbutaline)
- Magnesium sulfate
- Calcium channel blockers (such as nifedipine) and
- Non-steroidal anti-inflammatory drugs or NSAIDs (such as indomethacin)
Along with tocolytic medications, the primary step includes bed rest, painkillers, extra fluids, and adequate screening. In case the contractions do not subside, doctors continue administrating tocolytic medications depending on the risk measurement of having a preterm delivery. Transvaginal ultrasound and fetal fibronectin test can help you determine the risk of preterm delivery.
If the doctor decides to continue with tocolytics, the choice and dosage of the tocolytic drug are based upon the age of the baby and the condition of the baby’s lungs.
When Should You Not Use Tocolytics Medications?

Do not use these medications under the following conditions of your pregnancy:
- If the fetus is more than 34 weeks gestation
- If the fetus is less than 2500 grams or if it has placental insufficiency or IUGR (intrauterine growth restriction)
- When fatal chromosomal or congenital abnormalities are present
- If cervical dilatation is more than 6 centimeters
- If intrauterine infection or chorioamnionitis is present
- When fetal distress is present or suspected
- If the mother has eclampsia, preeclampsia, pregnancy-induced hypertension (PIH), vaginal bleeding, abruption placenta, cardiac ailment, etc.
- The baby has an abnormal heart rate
- If the baby has a slow growth rate
Side Effects Of Tocolytics
The side effects of tocolytics include:
Beta-Adrenergic Receptor-agonists (Terbutaline)
Hypotension, tachycardia, shortness of breath, chest pain, pulmonary edema, hypokalemia, hyperglycemia, etc are side effects of tocolytic agent Terbutaline
Magnesium Sulphate
When magnesium sulfate is used as a tocolytic agent, it can cause the pregnant woman to suffer from nausea, flushing, headache, lethargy, and hypotension
Nitric Oxide Donors (nitroglycerin)
This labor represent can cause flushing, tachycardia, hypotension, headache, and worsening of dependent cardiac lesions
Calcium Channel Blockers (Nifedipine)
Dizziness, flushing, hypotension are the side effects of using Nifedipine. However, if used with magnesium sulfate, it can suppress the heart rate, decrease contractility, cause an increase in hepatic enzyme levels
Cyclooxygenase Inhibitors (Indomethacin)
Nausea, GERD, gastritis, platelet dysfunction are all the side effects of Indomethacin
Oxytocin-receptor Antagonists
Hypersensitivity reactions and a probable increase in the fetal death
Tocolytic medicines should be used only if the risks are lesser than the benefits. In case the fetus dies in the womb or has some fatal abnormality that can cause death after delivery, doctors refrain from giving tocolytics to the mother.

Editorial Team,
With a rich experience in pregnancy and parenting, our team of experts create insightful, well-curated, and easy-to-read content for our to-be-parents and parents at all stages of parenting.Read more.
Responses (0)
Want curated content sharply tailored for your exact stage of parenting?
Related articles

Cervical Ripening During Labor – Is it Necessary, Methods Used and Tips to Prepare

Eel During Pregnancy – Is it Safe, Benefits and Side Effects

Itchy Feet During Pregnancy – Causes, Symptoms And Treatment

Vaginal Examinations During Labor – Importance, Frequency and Types

Pranayama During Pregnancy – Importance & Benefits
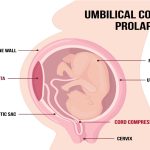
Umbilical Cord Prolapse – Causes And Tips To Manage
Sponsored content
Discover great local businesses around you for your kids.
Get regular updates, great recommendations and other right stuff at the right time.





